3 Powerful Strategies for Successful Reconditioning
By: Mike Potenza
One of the aspects of my role within our performance system is to manage the injury reconditioning training of our athletes.
I have come to enjoy working on these cases because of the complexity and the responsibility of coordinating a return-to-sport process that integrates the medical staff, performance staff and coaching staff.
A successful rehab and return to sport model can only be achieved through clear communication of the team personnel listed above. When breakdowns in communication occur, the athlete’s progress suffers.
Here are 3 of the most important lessons I’ve learned over the last 14 years when working with injured athletes:
Address Arthrogenic Muscle Inhibition (AMI)
The first rule I learned in my education on reconditioning and rehab was to address the disuse atrophy of the injured tissue. The phenomenon called Arthrogenic Muscle Inhibition (AMI) is caused by neurological shut down of the musculature surrounding an injury site. This causes a substantial decrease in muscle activation, reduces strength capabilities and promotes atrophy.
The science made complete sense to me, and I thought the best strategy to combat AMI would be appropriate exercise selection, volume and time under tension. However, I found that this approach would only take me so far, and with complex injury cases it slowed my progression to a crawl. I needed a strategy to jumpstart the muscles that had been dormant, weak and malfunctioning.
I found the answer when I was introduced to Bill Knowles who is the President of Knowles Athletic and a consultant for Athletic Development and Reconditioning for the Philadelphia Union Academy. Bill’s approach to rehab / reconditioning is unique and outside the box to say the least.
Knowing Bill’s experience level and education with injured athletes, I immediately consulted with him on my first ACL case in 2007, which was a tremendous learning experience!
During this ACL case my athlete was continuing to experience patella femoral pain as far out as 3 months post-op. The patella femoral pain restricted my exercise selection, and simultaneously limited my athlete’s quad development, thus slowing our return to sport plan.
Bill introduced me to the COMPEX muscle stimulation unit and how he integrated it’s use into his reconditioning programing, and later stage lower body strength training.
It was a game changer for me. The unit had a profound effect on recruiting motor units and their ability to turn on the muscle tissue to combat AMI.
The below exercise-progression is an example of how I’ve used the COMPEX during a post-surgical lower body reconditioning program.
Please keep in mind that you can use the device for an unlimited number of exercises, but it’s essential to first become familiar with the device’s programs and intensity levels to select the most appropriate use for the athlete’s current stage of rehab/reconditioning.
- Restricted isometric quad
- Limited ROM exercises like height restricted step-ups
- Body weight squats to progressive depths
- Single-leg squat variations
- Bi-Lateral, frontal plane movement on a “Skiers Edge”
- Recovery protocols to help with the reduction of edema
Integrate Assessments/Tests to Guide Programming
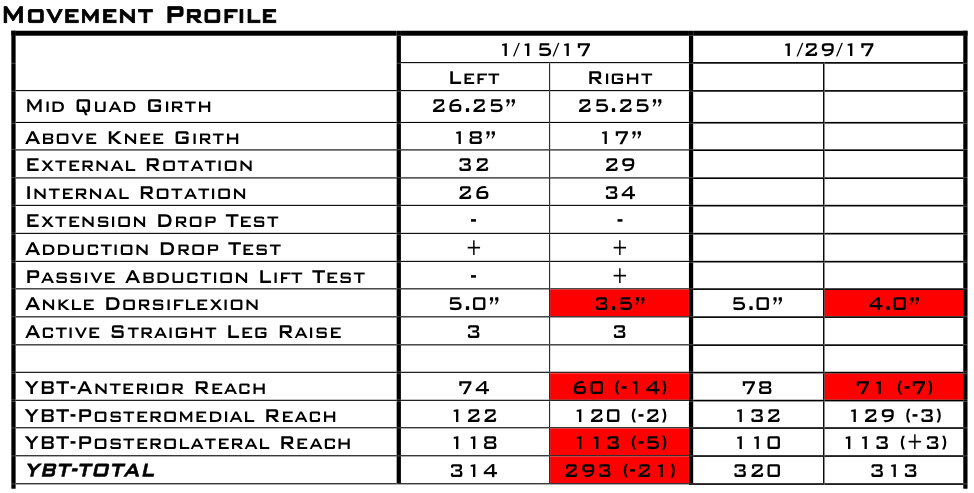
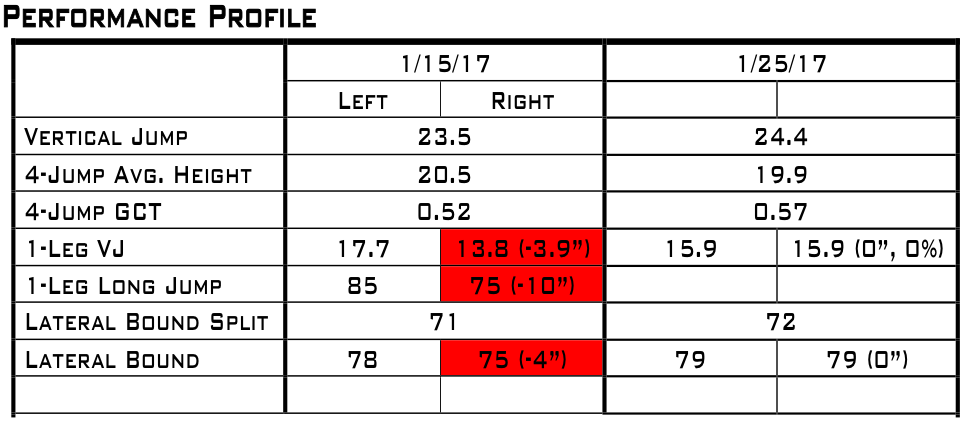
One of the most important tools I have to communicate with our coaches, management and scouting staff is testing results from our movement and performance profiling process.
The results not only measure the current physical capabilities of our team, but they also highlight the year to year progressions/regressions of our players. This information can help determine which physical performance quality or movement pattern needs improvement in order to best help optimize the athlete’s performance and durability.
Historical performance information becomes extra valuable when you have a long-term injury case. You can use prior testing information to set goals for the player to reach upon return to sport, as well as set benchmarks along the reconditioning plan based on percentages of performance bests. This is valuable both to monitor the effectiveness of the reconditioning program, and for the athlete’s psychology, as it allows them to objectively recognize their progress.
One of the most impactful areas of tracking movement capabilities and performance tests is that it has given me a clear vision on the programming direction I need to take with an injured athlete during a return to sport program.
Below is a sample of what we track during a lower body injury case and how we compare it to baseline scores.
Program Sport Progressions into the Reconditioning Plan
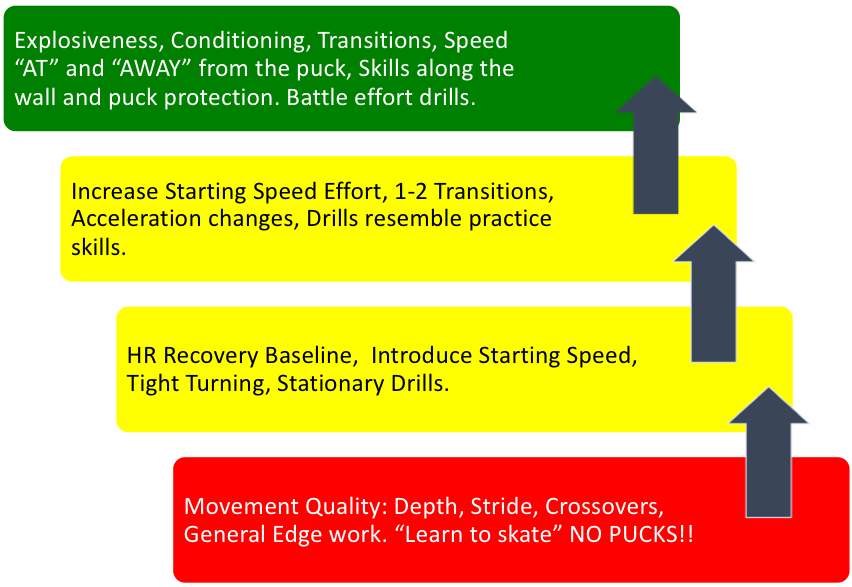
Once the athlete is ready to return to the ice, field, court or pool, there should be a structured plan ready with appropriate progressions. Much like designing a training program, it’s important to begin with the end in mind.
The “destination” is full participation with the team, in a controlled practice setting. Once the athlete can live and work in that environment, uninterrupted, then the coaching staff can make the determination when the player is game ready.
When I formulate the most effective path for a sport reintegration program, I keep strict adherence to the following rules:
- Pain free participation.
- Training does not go away with the introduction of the sport reintegration phase!
- Strict time frame for sport sessions.
- Follow a progression for drills in terms of movement patterns, intensity, skills and tactics.
- MOST OF ALL…..DON’T RUSH the reconditioning / rehab process.
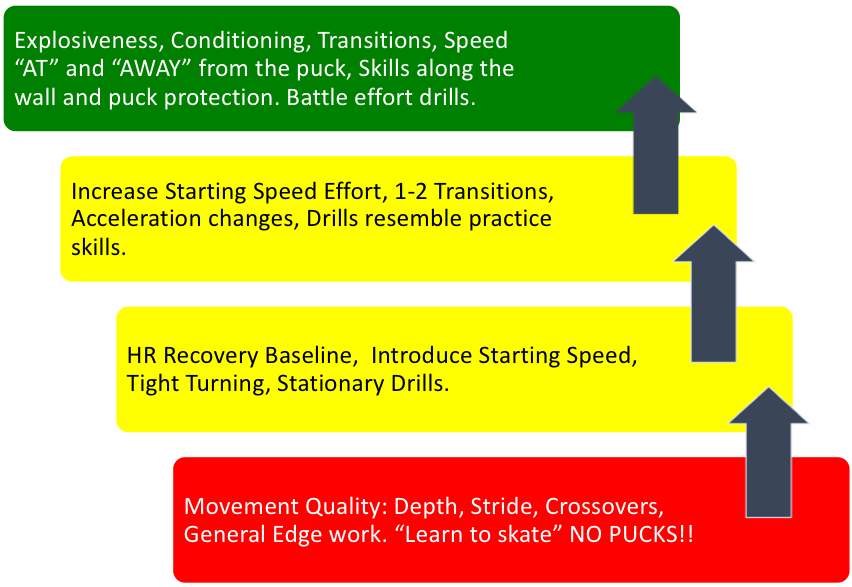
Below is an example of an Ice Hockey players return to ice progression after major knee surgery.
Wrapping Up
Athletes put trust in our profession to enhance performance through physical preparation, nutrition advice and recovery education. A hidden responsibility of our role as performance coaches is to aid in the rehabilitation/reconditioning process with the injured athlete. Understanding the barriers and limitations to training that the injured athlete faces will allow you to prescribe a highly effective and appropriate exercise program for their return. Be sure to benchmark and track the reconditioning process so that the athletes can build confidence from improved performances. The final step for a return to sport progression is to plan on-court / on-field controlled practice that prescribes drills that move from simple to complex, have controlled time frames and controlled intensities. Following these steps allows the athlete to make a successful transition back to competition and protects them from recurrences and flare-ups, which ultimately benefits both the player and the team.
Mike Potenza
Interested in learning more? Check out Optimizing Adaptation & Performance, a new video series from Mike Potenza, Kevin Neeld, and James LaValle that outlines the most effective strategies to maximize health, training progress and sport performance (available at a $50 discount for a limited time).

0 Comments for “3 Powerful Strategies for Successful Reconditioning”